Credentialing
What is Provider Credentialing?
Provider credentialing, also known as practitioner credentialing, is the process of verifying the qualifications, training, and professional background of healthcare providers. This process is essential for ensuring patient safety, operational efficiency, and compliance with industry standards.
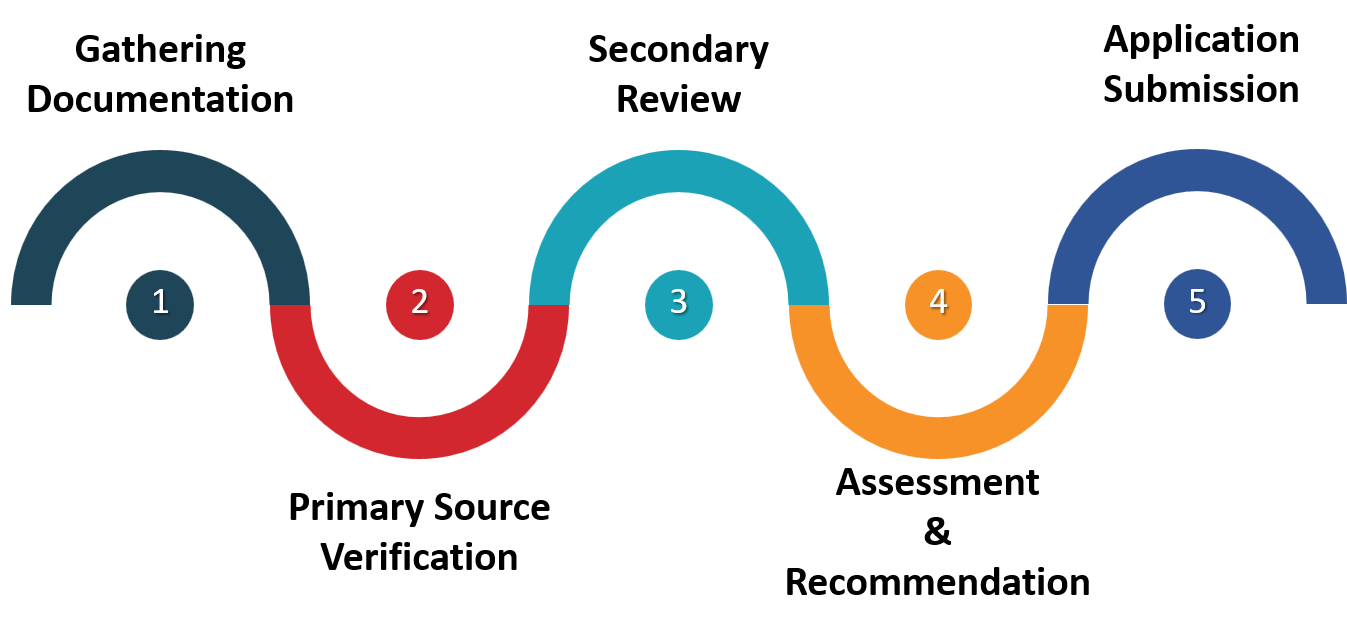
Steps in the Provider Credentialing Process
Initial Application Review
Collect and review the initial application to ensure all required information is included. This includes personal details, educational background, training, work history, and references
Gathering Documentation
Collect and organize essential credentials, licenses, supporting documents, and signatures required for provider enrolment. This may include:
- Proof of education (diplomas, transcripts)
- Licenses and certifications
- National Provider Identifier (NPI)
- Malpractice insurance coverage
- Professional references
- Detailed work history
- Background checks for disciplinary actions or legal issues
- State medical licenses
- DEA certificates
- Board certifications
- Educational transcripts
- Work history and references
Primary Source Verification (PSV)
Verify credentials directly with the issuing institutions, such as medical schools, residency programs, and licensing boards. This step confirms the authenticity of the applicant’s qualifications and is critical to prevent inaccuracies or fabrications.
Secondary Review
Conduct a thorough secondary review to identify any discrepancies or missing information from the initial application. This may involve cross-referencing details and following up on any inconsistencies.
Assessment and Recommendation
Assess and identify gaps, discrepancies, or red flags in the application. Make recommendations regarding credentialing, whether for enrolment with a payer or for consideration of clinical privileges1.
Application Submission
Submit the application to the insurance company or government payer, providing detailed information about the practice, credentials, and qualifications.
Review and Approval/Denial
The credentialing committee reviews the application and decides that aligns with the network’s credentialing policies and procedures, as well as the needs of patients. The application can be approved, denied, or require further review.
Updates and Maintenance
After initial enrolment, providers must maintain their status by updating their information regularly and complying with all payer requirements. This includes periodic recredentialing and updates to CAQH profiles.
Types of Credentialing
Facility Credentialing
Hospitals and other healthcare facilities perform a hospital credentialing process to authorize providers to practice at their facility.
Payer Credentialing
Insurance companies use payer credentialing to verify that providers meet their standards before allowing them to join their network, ensuring smooth reimbursement processes.